A Purple Blue Bump on Child’s Gum (Eruption Cyst/ Eruption Hematoma)
 Many parents sometime will find that their child or baby have a bluish-purple bump on their gingiva (gum). There is no need to panic, this is a fairly common development and is known as an eruption cyst or eruption hematoma.
Many parents sometime will find that their child or baby have a bluish-purple bump on their gingiva (gum). There is no need to panic, this is a fairly common development and is known as an eruption cyst or eruption hematoma.
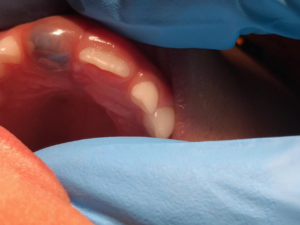 Children’s teeth form inside of a protective enclosure. As the teeth form, they move through the bone and then through the gums until they make it into the mouth. An eruption cyst occurs during the tooth’s final entry into the mouth, just under the surface of the gums. The protective enclosure around the teeth may leak fluid causing accumulation between the tooth and gum tissues. An opposing tooth due to bite force can also cause fluid and possible blood to accumulate. The color of the tissue around the tooth is dependent on the amount of blood that accumulates. The gum tissue can be swollen and appear to be a translucent color, bluish purple, or even dark red and brown. Although the eruption cyst or eruption hematoma are unattractive and often cause parents to worry, most are actually painless.
Children’s teeth form inside of a protective enclosure. As the teeth form, they move through the bone and then through the gums until they make it into the mouth. An eruption cyst occurs during the tooth’s final entry into the mouth, just under the surface of the gums. The protective enclosure around the teeth may leak fluid causing accumulation between the tooth and gum tissues. An opposing tooth due to bite force can also cause fluid and possible blood to accumulate. The color of the tissue around the tooth is dependent on the amount of blood that accumulates. The gum tissue can be swollen and appear to be a translucent color, bluish purple, or even dark red and brown. Although the eruption cyst or eruption hematoma are unattractive and often cause parents to worry, most are actually painless.
How are Eruption Cysts Treated?
Most of these hematomas will not require any special treatment. The tooth will break through the hematoma and emerge just like any normal teething experience. The broken tissue will heal on its own and probably won’t even cause any discomfort. Should parents have any concerns regarding the cyst they shouldn’t hesitate to call their pediatric dentist. Parents should describe the appearance, the time they noticed its presence, and any symptoms. The pediatric dentist will instruct as to whether or not the child should be seen in office. Occasionally, the excess fluid from the eruption cyst may stop the tooth from emerging through the gum. Rarely, a minor procedure under local anesthesia might be necessary to expose the tooth and allow complete eruption.
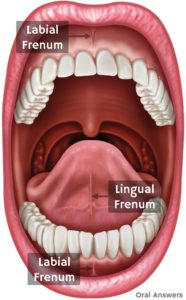 The tongue and lips are attached to the gingiva by a muscular attachment called a frenum. There are two frena (the plural form of frenum) in the mouth. 1. Lingual frenum, which connects the tongue to the floor of the mouth, and the 2. maxillary labial frenum, which connects the inside of your upper lip to your gums just above the upper two front teeth. These frena can sometimes prevent normal function or create pain. Surgical removal of the frenum is called a frenectomy. Today, laser dentistry offer a more comfortable treatment alternative to use of surgical scalpel (blade) with minimal local anesthesia and bleeding, and without the need for sutures (stitches).
The tongue and lips are attached to the gingiva by a muscular attachment called a frenum. There are two frena (the plural form of frenum) in the mouth. 1. Lingual frenum, which connects the tongue to the floor of the mouth, and the 2. maxillary labial frenum, which connects the inside of your upper lip to your gums just above the upper two front teeth. These frena can sometimes prevent normal function or create pain. Surgical removal of the frenum is called a frenectomy. Today, laser dentistry offer a more comfortable treatment alternative to use of surgical scalpel (blade) with minimal local anesthesia and bleeding, and without the need for sutures (stitches). Sometimes, the lingual frenum can cause a condition called ankyloglossia or “tongue-tie” which occurs when the attachment runs all the way to the tip of the tongue causing restrictive protrusion of the tongue. Children are able to accommodate well to a restrictive lingual frenum and can eat and speak normally. If the attachment causes abnormal function such as speech impairment, breastfeeding problem in infants (poor latch) then a lingual frenectomy may be necessary to give the child normal tongue function and feeding.
Sometimes, the lingual frenum can cause a condition called ankyloglossia or “tongue-tie” which occurs when the attachment runs all the way to the tip of the tongue causing restrictive protrusion of the tongue. Children are able to accommodate well to a restrictive lingual frenum and can eat and speak normally. If the attachment causes abnormal function such as speech impairment, breastfeeding problem in infants (poor latch) then a lingual frenectomy may be necessary to give the child normal tongue function and feeding. Sealant is a white or clear plastic material that is applied to the biting (depression and grooves) surfaces of the back permanent teeth. The sealant acts as a barrier, protecting the decay-prone areas of the back teeth from plaque and acid. Although thorough brushing and flossing can remove food particles and plaque from smooth surfaces of teeth, they cannot always get into all the nooks and crannies of the back teeth to keep them clean. Sealant protects these vulnerable areas from tooth decay by “sealing out” plaque and food.
Sealant is a white or clear plastic material that is applied to the biting (depression and grooves) surfaces of the back permanent teeth. The sealant acts as a barrier, protecting the decay-prone areas of the back teeth from plaque and acid. Although thorough brushing and flossing can remove food particles and plaque from smooth surfaces of teeth, they cannot always get into all the nooks and crannies of the back teeth to keep them clean. Sealant protects these vulnerable areas from tooth decay by “sealing out” plaque and food. The American Academy of Pediatric Dentistry recommends the use of fluoride toothpaste at the first sign of tooth eruption using only a smear of tooth paste. The recommended toothpaste is one that has the ADA seal.
The American Academy of Pediatric Dentistry recommends the use of fluoride toothpaste at the first sign of tooth eruption using only a smear of tooth paste. The recommended toothpaste is one that has the ADA seal. While fluoride is a naturally occurring compound, it can still cause side effects when consumed in large doses. In 2015, the U.S. Department of Health and Human Services (HHS) released its recommendation lowering the optimal concentration of fluoride to 0.7 mg per liter of water from the previous 1962 of 1.2 mg per liter.
While fluoride is a naturally occurring compound, it can still cause side effects when consumed in large doses. In 2015, the U.S. Department of Health and Human Services (HHS) released its recommendation lowering the optimal concentration of fluoride to 0.7 mg per liter of water from the previous 1962 of 1.2 mg per liter. The American Academy of Pediatric Dentistry recommends a tiny smear of fluoridated toothpaste to be used for children under the age of 2. The illustration shows the incorrect amount of toothpaste for a child. This amount could be swallowed by the child increasing or exceeding the daily amount necessary. A pea-sized amount is recommended for children under six years of age. You should also keep it out of reach; kids are sometimes tempted to eat toothpaste.
The American Academy of Pediatric Dentistry recommends a tiny smear of fluoridated toothpaste to be used for children under the age of 2. The illustration shows the incorrect amount of toothpaste for a child. This amount could be swallowed by the child increasing or exceeding the daily amount necessary. A pea-sized amount is recommended for children under six years of age. You should also keep it out of reach; kids are sometimes tempted to eat toothpaste. Dental radiographs serve as an adjunct to the dentist’s in best diagnosis and treatment. The American Dental Association (ADA) encourages dentists and patients to discuss dental treatment recommendations, including the need for X-rays, to make an informed decision together. Radiation exposure associated with dentistry represents a minor contribution to the total exposure from all sources, including natural and man-made.
Dental radiographs serve as an adjunct to the dentist’s in best diagnosis and treatment. The American Dental Association (ADA) encourages dentists and patients to discuss dental treatment recommendations, including the need for X-rays, to make an informed decision together. Radiation exposure associated with dentistry represents a minor contribution to the total exposure from all sources, including natural and man-made. Most injuries to primary teeth occur at 18 – 30 months of age, the toddler stage. As they learn to walk, they may fall forward landing on their hand and knees. The teeth most frequently injured are the upper central incisors, especially with protruding teeth being two to three times more prone. There are various types of injuries:
Most injuries to primary teeth occur at 18 – 30 months of age, the toddler stage. As they learn to walk, they may fall forward landing on their hand and knees. The teeth most frequently injured are the upper central incisors, especially with protruding teeth being two to three times more prone. There are various types of injuries: